Bringing Safe Patient Handling & Mobility (SPHM)
to the Public Health Forefront
Sasha M. Latvala, BS, CSPHP – United States
When many of us think about public health, we envision preventing and tracking diseases, including outbreaks. Others may view it as promoting and improving community health, particularly of minority or underserved populations. While both are correct, public health encompasses a wide range of areas, such as setting the standards that ensure the safety and protection of workers. Those within the occupational health and safety community work diligently to prevent work-related illness, injury, disability, and even death from occurring. So where and how does SPHM fit in?
The Role of SPHM within Public Health:
Mitigating Risk:
SPHM practitioners focus their efforts on mitigating risk and preventing injuries to healthcare workers and their patients using a variety of elements:
- Education and training
- Work design
- Preventative controls (i.e., SPHM technology, assessment tools)
- Policy and/or legislative measures
- Advocacy and outreach
- Research
These elements are intricately woven through workplace-based initiatives such as SPHM programming. SPHM programs are comprehensive interventions that have demonstrated their effectiveness in injury reduction. However, does this type of approach further highlight the Inequality Paradox? 2
Gaps within SPHM Research:
Social determinants of health are non-medical factors that can significantly influence healthy outcomes behaviors and the quality of life within a population. They include many different aspects within various environments that an individual is exposed to.
While the data may indicate that nurses and nurse assistants are more likely to incur a musculoskeletal disorder due to the demanding physical nature of their work and the tremendous stress it puts on the human body, it has not been thoroughly explored if there are further underlying determinants that contribute to what we have seen thus far in the research. By investigating how factors such as income, stress, health literacy, housing, and language can further impact the injuries we see among nurses and nurse assistants, we can learn to refine our interventions to better mitigate risk and improve overall well-being and quality of life.

Source: Centers for Disease Control
In 2019, Sabbath et al published a study within the American Journal of Public Health that explored whether or not there was an injury rate disparity between higher-wage workers and lower-wage workers when applying a patient handling intervention.5 This study was one of the first to empirically examine whether socioeconomic status shapes the effectiveness of occupational health interventions, and underscores the importance of why more research such as this is needed within the SPHM industry. This research came out of 1 of the 6 Centers of Excellence for Total Worker Health™, the Center for Work, Health and Well-Being, and was spearheaded by the Harvard T.H. Chan School of Public Health.
Total Worker Health™
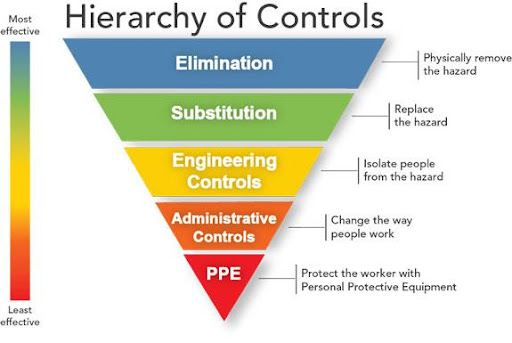
Source: National Institute of Occupational Safety and Health
Hierarchy of Controls Applied to NIOSH Total Worker Health™
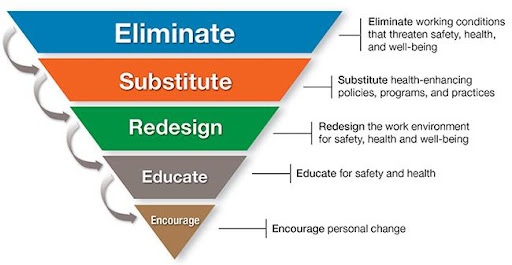
Source: National Institute of Occupational Safety and Health
Conclusion:
The field of SPHM has evolved drastically over the past two decades in terms of technology, advocacy, and awareness within the public arena. Nonetheless, much more work is needed with respect to research, particularly in the context of social determinants of health. The data we derive from this research can ultimately assist us with our interventions, policy, and legislative measures. SPHM practitioners are encouraged to advocate for further advances in research in an effort to ignite meaningful dialogue and to demonstrate a shared commitment to promoting the health, safety, and well-being of healthcare workers.
References:
[1] Waters TR. When is it safe to manually lift a patient? American Journal of Nursing. 2007; 107(8):53-59. doi:10.1097/01.NAJ.0000282296.18688.b1
[2] Frohlich KL, Potvin L. Transcending the known in public health practice: The inequality paradox: the population approach and vulnerable populations. Am J Public Health. 2008;98(2):216-221. doi:10.2105/AJPH.2007.114777
[3] Work Injury Source. Workplace Injury Statistics—2020 Data for Workplace Accidents, Injuries and Deaths. Work Injuries. Updated January 22, 2021. Accessed March 15, 2021.
[4] U.S. Bureau of Labor Statistics. Injuries, Illnesses and Fataltities. Accessed January 30, 2021.
[5] Sabbath EL, Yang J, Dennerlein JT, Boden LI, Hashimoto D, Sorensen G. Paradoxical impact of a patient handling intervention on injury rate disparity among hospital workers. Am J Public Health. 2019;109(4):618-625. doi:10.2105/AJPH.2018.304929
[6] National Institute of Occupational Safety and Health (NIOSH). Fundamentals of total worker health approaches: Essential elements for advancing worker safety, health, and well-being. By Lee MP, Hudson H, Richards R, Chang CC, Chosewood LC, Schill AL, on behalf of the NIOSH Office for Total Worker Health. Cincinnati, OH: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health; 2016.